Just A Head Tilt Or Torticollis The Importance Of Early Referral
July 04, 2022


Are they shy or is it Torticollis?
What is Torticollis?
In a Torticollis diagnosis, the sternocleidomastoid muscle of the cervical spine becomes abnormally contracted, resulting in ipsilateral lateral flexion and contralateral rotation of the cervical spine. This causes head tilting to one side, while the chin rotates to the opposite side.
Two subtypes: congenital and acquired.
Most cases of torticollis can be acquired and correlated with some type of craniofacial asymmetry, (plagiocephaly, frontal bossing, etc.). Torticollis is commonly seen in at least 1 in 300 births, however, the incidence has increased since the “back to sleep” campaign was implemented. Torticollis is mostly present on the right side and up to 20% of patients will also have developmental dysplasia of the hip (DDH).
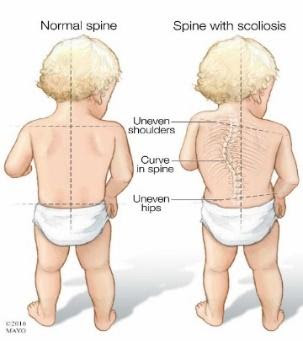
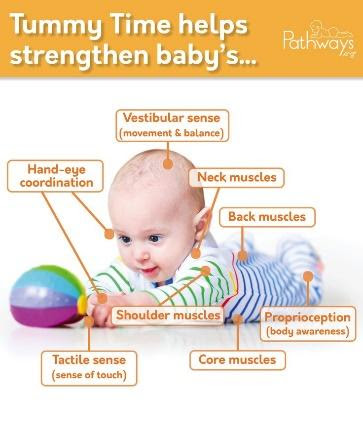
Left untreated, torticollis can result in asymmetrical strength, decreased bimanual skills, feeding challenges, visual impairments, sensory processing impairments, postural impairments and developmental delays.


Symptoms
- Visible cervical lateral flexion with chin rotation towards the opposite side
- Muscular tightness upon cervical flexion and rotation
- Difficulty nursing from one side
- Preference to look to one side in all positions
- Flatness on cranial structures
- Visible red creases on the skin of the neck
- Early head preference and developmental delays.
Congenital torticollis is related to positioning in utero, breech presentation, twin pregnancies, and newborns with body length of more than 51.3+1.49 cm, tongue or lip ties and prolonged NICU stays. Other factors include neurological or genetic conditions and injuries (stroke, syndromes, brachial plexus injury. Etc.).
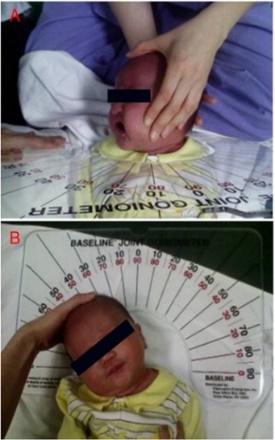
Diagnosis
The diagnosis of torticollis is primarily clinical; although in some cases an x-ray will be ordered to rule out structural deformities. An ultrasound is helpful as well to check for the presence of a congenital tumor associated with torticollis called fibromatosis coli.
Postural compensations that are commonly seen in children with torticollis include shoulder hiking, hip hiking (tripod crawling), and uneven weight bearing while sitting and standing. If these postural compensations are not addressed, they can further lead to scoliosis and asymmetrical strength.
Other aspects about torticollis to keep in mind are underlying tongue and lip ties which can lead to temporal-mandibular joint dysfunction or visual or hearing impairments resulting in head tilting.



Impact of early referral
In the past, referrals to torticollis specialists weren’t made until significant postural impairments were already noted. Today, we have more available research and guidance from various organizations highlighting the importance of early diagnosis and Physical Therapy referral, starting from infancy, to achieve full torticollis resolution and avoid secondary torticollis-related impairments.
The American Physical Therapy Association completed a literature review and highlighted the correlation between age of referral, length of time of treatment intervention and gains in range of motion of the cervical spine with the following results:
- PT initiated at 1 month of age = resulted in 1.5 months of PT required to achieve 98% of gains in range
- PT initiated at 1-3 months of age = resulted in 6 months of PT required to achieve 89% of gains in range
- PT initiated at 3-6 months of age = resulted in 7 months of PT required to achieve 62% of gains in range
- PT initiated at over 6 months of age = resulted in 6 months of PT required to achieve <20% of gains in range
Biggest gains: birth to 3 months
Research shows that most gains will be achieved when infants are referred to therapy from birth to 3 months. This also results in shorter episodes of care. An early physical therapy referral also provides the opportunity to perform conservative treatment before referring to a specialist who may recommend a more invasive treatment approach such as Botox or surgical lengthening.
It is key to consider that earlier physical therapy intervention will allow for the monitoring of developmental milestones and feeding challenges to ensure there is resolution of torticollis and whether a referral to a specialist is necessary.
Research has concluded that 90-99% of cases of acquired torticollis can be corrected with conservative treatment via early detection and referral to Physical Therapy.
Well care physician strategies
Strategies that can be implemented during well care visits to evaluate for torticollis include:
- A thorough medical history and manual examination to identify infants with torticollis.
- Assessment of posture in supine, prone, sitting and standing to look for asymmetries.
- Incorporating cervical and shoulder range of motion assessments both passively and actively to help diagnose torticollis and to rule out other conditions.
Prevention tips to share with parents
As physicians, it is helpful to provide strategies for parents on how to prevent torticollis. These include:
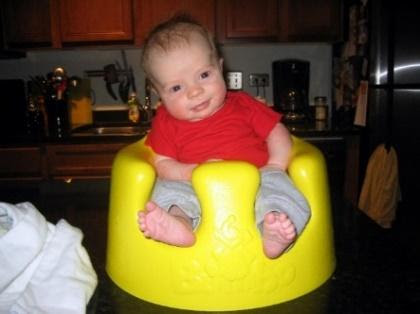
- Decreasing or avoiding time in devices such as bouncers, jumpers or walkers.
- Teaching proper positioning in car seats and strollers to make sure the child is positioned in midline.
- Taking infants out of the car seat or swing if they fall asleep and transferring them into a crib.
- Floor time, which is necessary for optimal development of fine and gross motor skills. Providing awake and supervised tummy time and laying the child on their right and left side to prevent positional plagiocephaly and facial asymmetries.
- Having the child actively track a toy placed on the left and right side while laying on their backs, during tummy time and sitting to ensure their cervical spine is turning both ways.
- During feeding, if a child is being bottle fed, make sure the caregiver switches sides in order to help the child look in both directions and switch sides during burping and when carrying a child.


Specialized Torticollis treatment
At Joe DiMaggio Children’s Hospital Outpatient Rehabilitation centers, our highly skilled physical therapists are specialized in Torticollis treatment interventions, including:
- Therapeutic exercises (active and passive)
- Gross and fine motor skill development
- Manual therapy
- Application of Kinesio tape
- Visual awareness strategies
- Caregiver education
Torticollis diagnosis, if treated in a timely manner, can be managed with conservative treatment and resolved in early childhood, through education and guidance from a dedicated physical therapist in collaboration with the team of physicians.
